Unspecified Anxiety Disorder Va Rating
anxiety disorder ratingA 10 rating requires. These ratings are based on the level of social and occupational impairment a veteran experiences and the severity of symptoms VA uses to characterize that impairment.
Dsm 5 Classification Criteria And Use Ppt Download
Panic disorder andor.
Unspecified anxiety disorder va rating. Unspecified anxiety disorder DC 9413. So the rating system is the same as that of other mental illnesses like anxiety disorders. Medical condition anxiety disorders.
For Reservists the condition must have occurred in or resulted from an injury in the Line of Duty to qualify. PTSD is the only anxiety disorder for which a. Do you get a rating for unspecified depressive disorder.
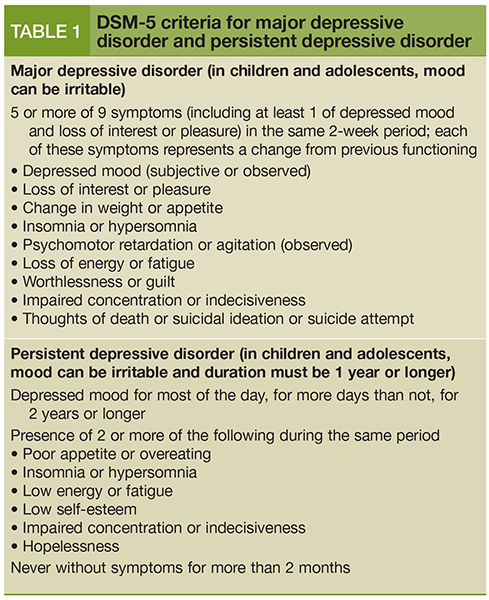
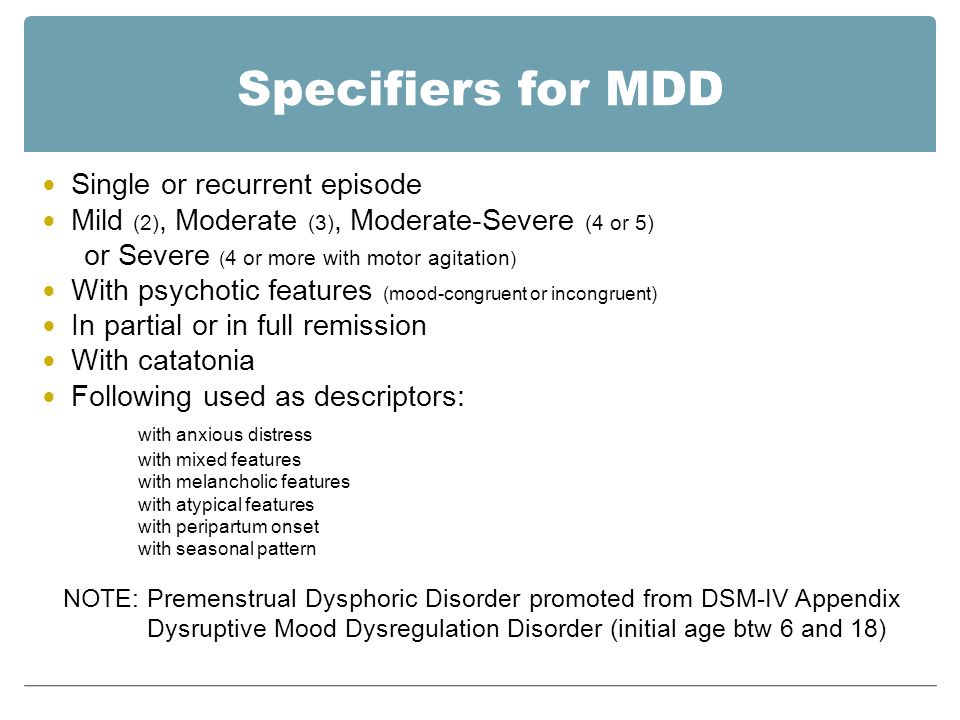
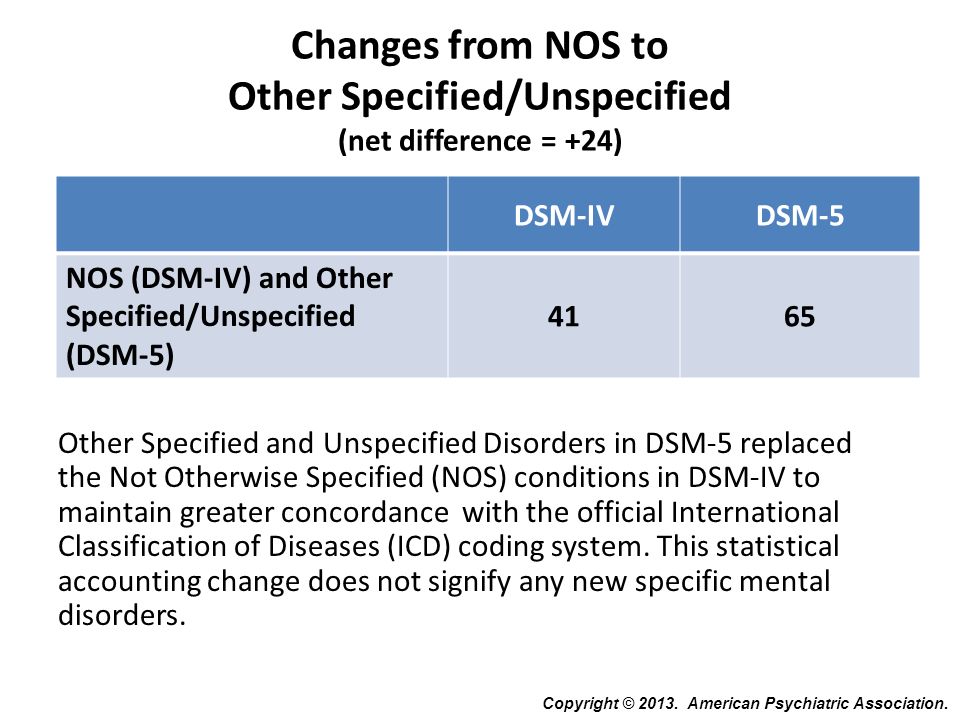
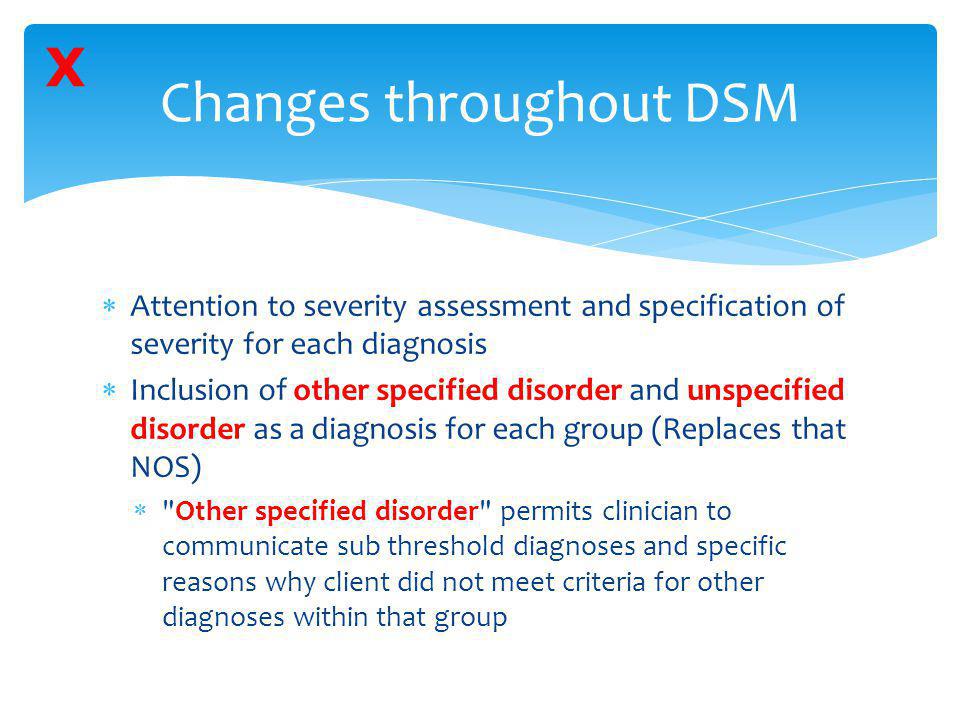
The VA awards disability compensation for each Mental Disorder that is service-connectedThe DoD will also rate service-connected Mental Disorders as long as they also make the service member Unfit for Duty. Depression falls under the General Rating Formula for Mental Disorders category on the rating schedule. Social phobia Obsessive compulsive disorder Other and unspecified neurosis Posttraumatic stress disorder Panic disorder andor agoraphobia Anxiety disorder not otherwise specified DISSOCIATIVE DISORDERS.
There are five levels of ratings from 0-100 in 10 percent increments that result in benefits. 9312 Major or mild neurocognitive disorder due to Alzheimers disease. The VA rates this mental illness based on how much it impairs the veterans occupational and social ability.
VA claims for PTSD and Depression are rated on the same general scale according to CFR 38 Part 4 Schedule for Rating Disabilities General Rating Formula for Mental Disorders. Generalized anxiety disorder 9400 Phobias and social anxiety disorder 9403 Obsessive-compulsive disorder 9404 Other specified anxiety disorder 9410 Post-traumatic stress disorder 9411 Panic. When rating service-connected anxiety disorders VA uses the General Rating Formula for Mental Disorders included in 38 CFR 4130 to assign one of the following percentages.
I was asking because at my CP I was diasnoged with that instead of PTSD. Anxiety disorder not otherwise specified. 9327 Removed 9400 Generalized anxiety disorder.
Mental Disorders are by far the most difficult medical conditions to rate. 9310 Unspecified neurocognitive disorder. In order to get a VA rating for PTSD and Depression you need to have 1 A medical diagnosis of both conditions with a separate diagnosis.
Other and unspecified neurosis. Organic mental disorder other including personality change due to a general. Posttraumatic stress disorder.
0 10 30 50 70 or 100. Scheduling of ratingsmental disorders ANXIETY DISORDERS 4130-2 Generalized anxiety disorder Specific simple phobia. 9326 Major or mild neurocognitive disorder due to another medical condition or substancemedication-induced major or mild neurocognitive disorder.
The average VA disability rating for anxiety is 70. The VAs diagnostic codes for anxiety disorders as well as other related disorders are as follows. As many as one in every three veterans suffer from depression anxiety adjustment disorder PTSD or other psychiatric disorder - two to three times more than the general population.
Ratings under diagnostic. Post Feb 04 2016 1 2016-02-04T1217. A non-compensable 0 percent rating indicates the veteran has a diagnosis of sleep apnea but the condition is asymptomatic.
Generalized anxiety disorder. Va Rating for Unspecified Depressive Disorder Va Rating for Unspecified Depressive Disorder. Depression is a major cause of unemployability in the US making VA disability compensation for depression extremely important.
Anxiety disorders are most commonly rated under CFR 38 Part 4 VA Schedule of Ratings Diagnostic Code 9400 Generalized Anxiety Disorder. Veterans are assigned either a 0 30 50 or 100 percent rating depending on the severity of their condition. The Department of Veterans Affairs VA is amending the portion of its Schedule for Rating Disabilities VASRD dealing with mental disorders and its adjudication regulations that define the term psychosis.
Within 4130 Schedule of Ratingsmental disorders of the VAs Schedule for Rating Disabilities Diagnostic Code 9400 is for Generalized Anxiety Disorder. Veterans in this post I break down the VA Rating for PTSD and Depression. A 30 percent rating is awarded when a veteran experiences chronic daytime sleepiness ie.
Yes anxiety is a VA disability and can be rated at 0 10 30 50 70 or 100 depending upon the frequency severity and duration of your symptoms. Obsessive compulsive disorder.