Va Disability Rating For Bilateral Plantar Fasciitis
bilateral disability fasciitis ratingFor Reservists the condition must have occurred in or resulted from an injury in the Line of Duty to qualify. REMANDED Entitlement to a disability rating higher than 10 percent for bilateral plantar fasciitis with left foot calcaneal spur is.
Finally consistent with other foot injuries and disabilities VA intends to include a note with DC 5285 that would instruct rating personnel to assign a 40 percent rating in cases where there is actual loss of use of the foot.

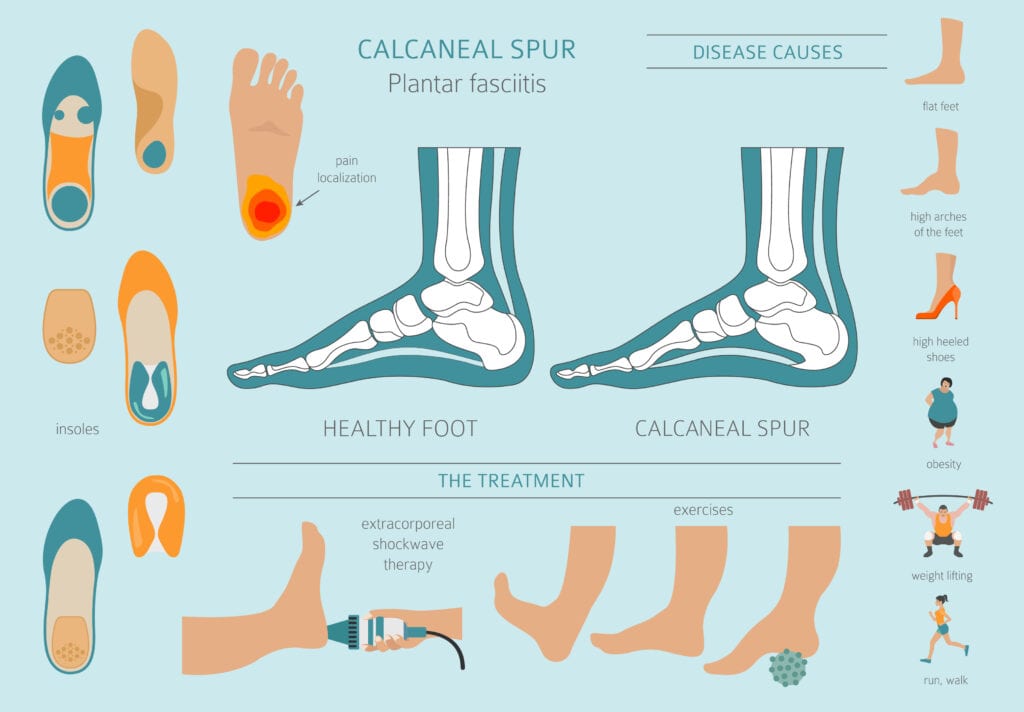
Va disability rating for bilateral plantar fasciitis. The VA awards disability compensation for each Foot condition that is service-connectedThe DoD will also rate service-connected conditions as long as they also make the service member Unfit for D uty. This condition is one of the most common causes of heel pain and involves inflammation of a thick band of tissue that runs across the bottom of the foot and connects the heel bone to the toes. If you have two conditions that are compensable in both your lower extremities or upper extremities you can receive an extra 10 percent factored into your combined disability rating.
If you have bilateral plantar fasciitis you could be eligible to receive a VA disability rating for foot pain of 50. Dec 26 2012 1. The most current disability rating and severity of symptoms can be found in the Code of Federal Regulations at 38 CFR 471 Schedule of ratings respiratory system.
If these elements are present and you have plantar fasciitis in one foot you may receive a disability rating of 30. I could probably get an increase if I applied but Im already rated 100 through other issues. Without the additional benefit for the bilateral factor calculation the veteran would have been stuck at 40.
VA changed the rating criteria in early 2021 adding a diagnostic code specifically for plantar fasciitis. VA math in Hutskys calculator comes out right if I enter this in on the bilateral side with 10. In looking at my rating letter I was awarded 10 for Plantar fasciitis with degenerative changes bilateral.
Yes Plantar Fasciitis is a VA disability and can be rated at 0 10 20 30 or 50 depending upon unilateral one foot versus bilateral both feet and the severity of your symptoms. I am 30 bilateral pes cavus wplantar fasciitis bilateral. Bilateral disabilities are recognized by VA as severely limiting to a veterans ability to function and thus warrant a higher rating percentage.
The claw footpes cavus leads to plantar fascittis pain and so on. In this particular example that extra 37 was just enough to push the overall combined rating increased to 50. Should I not have this awarded for each foot claim was for both feet and thus have this at 10 for each foot meaning 10 would be entered in the bilateral part of the spreadsheet twice.
Smooth says 50 so you can almost bank on the 30 for sure. Through the VA have done custom inserts cortisone shots flo graft shots and Dynasplint devices. What Evidence Will VA Require for My Disability Compensation Claim.
For an individual whose plantar fasciitis either unilateral or bilateral is responsive to treatment either non-surgical or surgical VA proposes a 10 percent disability rating. Marked pronation extreme tenderness of plantar surfaces of the feet marked inward displacement and severe spasm of the Achilles Tendon on. VA should round that 47 up to 50.
Basically Ive exhausted everything short of surgery. VA Disability Ratings for Shrapnel Wounds. Ask me anything Im pretty much an expert at this point about the VA and plantar fasciitis.
Plantar Fasciitis is most often rated analogous to CFR 38 Part 4 VA Schedule of Ratings Diagnostic Code 5276 Flatfoot Acquired. Both the VA and the DoD award Military Disability for the Foot. If you look at the rating charts they have a pretty descriptive breakdown.
Below are the specific qualifications for each rating percentage. 10 Veterans can receive the 10 percent rating for plantar fasciitis affecting one or both feet that is responsive to treatment.